Abstract
Introduction
Advances in chemotherapy regimens have greatly improved outcomes in acute leukemia (AL) with 5-year survival being 90% in acute lymphoblastic leukemia (ALL) and 60-70% in acute myeloid leukemia (AML). Despite these advances, AL accounts for the greatest proportion of malignancy-related death among children. We and other investigators have shown that this mortality burden, frequently in the context of infectious complications, is greater in racial minority groups. We sought to expand these prior analyses by using automated data extraction from the electronic medical record (EMR) combined with geocoded block group level estimates of poverty to examine the incidence of bloodstream infection during induction in relation to race and socioeconomic status (SES).
Methods
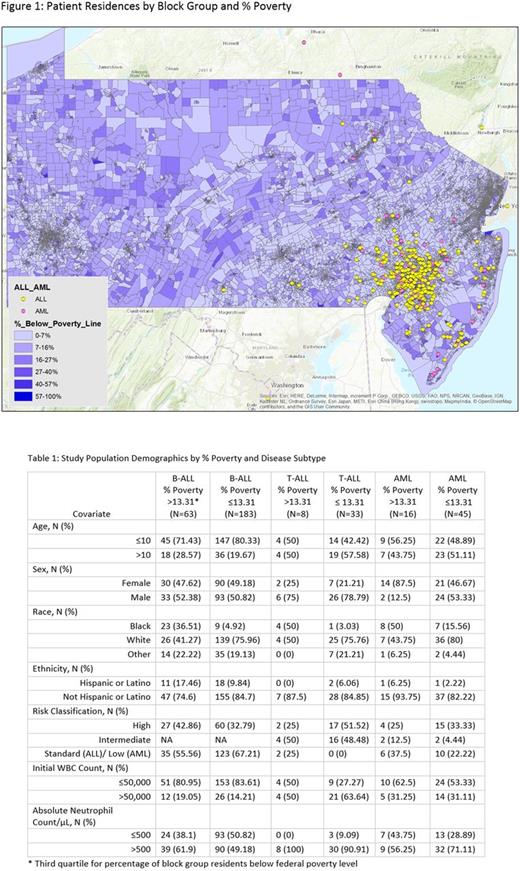
A total of 287 ALL (246 B-ALL, 41 T-ALL) and 61 AML patients who started therapy at The Children's Hospital of Philadelphia between 2006 and 2014 were included. Risk group, chemotherapy protocol, course dates, and initial white blood cell (WBC) count were manually abstracted into a REDCap database. Patient age, sex, race, blood culture results, initial absolute neutrophil count (ANC), and residential address were extracted from the EMR with an automated REDCap/EPIC data query tool. Residential addresses were batch-matched to geo-coordinates that linked each patient to a census-derived block group. Figure 1 shows patient residential address mapped onto the percentage of residents below the federal poverty level in each block group. Percent below poverty was dichotomized at greater than the third quartile (13.31%), as a measure of block group SES. Course level bloodstream infection incidence was computed based on positive blood culture results between course start and end dates. Common commensal organisms were only counted as true pathogens if there were two or more positive blood cultures for the same organism in a three day period. Log-binomial regression was used to compute the unadjusted risk ratios (RR) and corresponding 95% confidence intervals (CI) comparing incidence of bloodstream infection during induction by block group SES, race, sex, age, risk classification and presenting WBC and ANC. Due to the small number of T-ALL patients, T-ALL and B-ALL patients were grouped for modeling.
Results
Patient characteristics are shown in Table 1. The cumulative incidence for any bloodstream infection throughout the course of treatment was 82% for AML patients, and 18% and 24% for B-ALL and T-ALL patients, respectively. 52% of AML patients developed viridans group streptococcal bacteremia during the course of therapy, and 6% had fungemia, from organisms in the Candida, Trichosporon, or Fusarium genera. Incidence of any bloodstream infection during first induction was 5.88% for ALL and 16.13% for AML. In ALL patients, age >10 y (RR: 0.35 , 95% CI: 0.08, 1.51) and black race (RR: 0.75, 95% CI: 0.18, 3.18) were associated with a lower bloodstream infection risk during induction, whereas block group with >13.31% below poverty (RR: 1.27, 95% CI: 0.46, 3.47), females (RR: 1.38, 95% CI: 0.55, 3.47), high risk classification (RR: 1.67, 95% CI: 0.66, 4.18), presenting WBC >50,000 (RR: 3.03, 95% CI: 1.22, 7.53) and presenting ANC ≤500 (RR: 1.58, 0.63, 3.99) suggested a higher bloodstream infection risk during induction, though none of these associations achieved statistical significance. Results of similar magnitude and direction were obtained for AML with the exception of presenting ANC ≤500 (RR: 0.84, 95% CI: 0.24, 2.91).
Conclusions
This study demonstrates the feasibility of linking automatically extracted patient demographic and laboratory data with geocoded estimates of block group level covariates to evaluate the association between socioeconomic status and bloodstream infection risk during induction therapy among children with AL. Work is ongoing to expand the study population to other centers, to extend the bloodstream infection susceptibility analyses to other chemotherapy courses, and to evaluate event free and overall survival. This preliminary analysis suggests that race and poverty may have unexpectedly discrepant relationships with health outcomes. These findings suggest the need for larger studies to better parse the independent effects of race and SES, as well as their potential interaction, on incident bloodstream infection in pediatric AL.
Fisher: Merck: Research Funding; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal